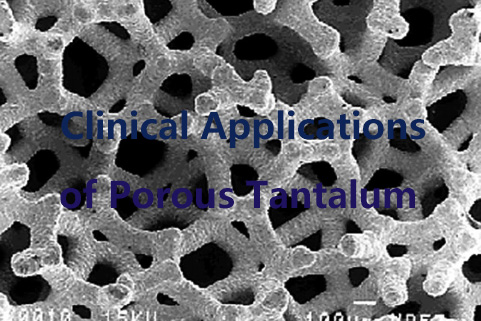
Clinical Applications of Porous Tantalum
Porous tantalum has emerged as a valuable material in biomedical engineering due to its high biocompatibility, corrosion resistance, and mechanical properties that closely resemble those of natural bone. Initially synthesised for orthopaedics, its applications have expanded to include dentistry, cardiovascular devices, and experimental regenerative medicine. This document outlines its experimental and clinical applications.
 [1]
[1]
Why Porous Tantalum?
Tantalum is a refractory metal that possesses numerous advantages when used as a biomaterial. Porous tantalum is particularly desirable for osseointegration and long-term biological stability.
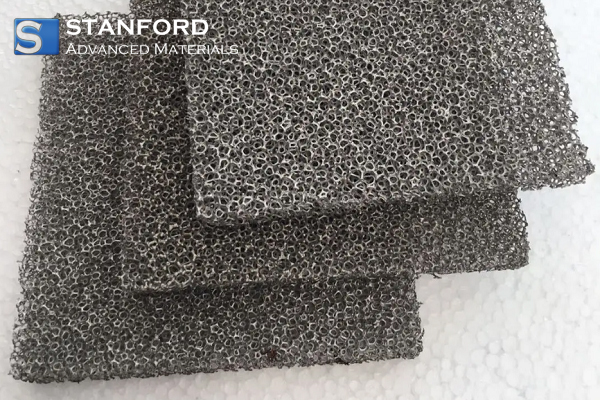
Porous tantalum is produced by depositing tantalum onto a scaffold, resulting in a highly uniform, interconnected structure suitable for medical implants. Tantalum foam, created through sintering or space-holder methods, typically has a less regular pore structure and is generally used in structural or experimental applications where lower precision is acceptable.
Porous tantalum possesses several significant properties that are ideal for biomedical applications.
- High porosity, reaching up to 80%, allowing for tissue ingrowth and vascularisation.
- Its elastic modulus is very similar to that of cancellous bone, thereby reducing stress shielding and promoting natural load transmission.
- Porous tantalum has excellent corrosion resistance, maintaining stability and inertness under physiological conditions.
- Its high friction coefficient ensures maximum initial mechanical stability upon implantation.
These characteristics make porous tantalum particularly well-suited for load-bearing implants and tissue engineering scaffolds.
Further reading: Tantalum: Properties and Applications
 [2]
[2]
1. Orthopaedic Implants
Porous tantalum is extensively employed in orthopaedic reconstructive surgery, especially for patients with significant bone loss or poor bone quality.
--Hip and Knee Arthroplasty with Porous Tantalum
Porous tantalum has proven effective in complex hip and knee arthroplasty procedures. Its mechanical stability combined with high bone ingrowth potential is particularly beneficial in revision total hip arthroplasty (THA) and total knee arthroplasties.
In revision THA, porous tantalum modular augments and acetabular cups are increasingly used to address extensive bone loss and complex acetabular defects. These implants feature a highly porous surface that facilitates rapid bone ingrowth, and their high friction coefficient allows for strong primary fixation.
A notable clinical study by Weeden and Schmidt (2008) reported a 98% survivorship rate at five years for patients who received porous tantalum acetabular cups during revision THA. The study examined 43 complicated acetabular revisions, including 33 Paprosky type 3A and 10 type 3B defects with significant host bone loss and pelvic discontinuity. Modular tantalum augments were employed to complement the acetabular shell in 26 cases. At an average follow-up of 2.8 years, 42 of 43 components remained stable, with one failure attributed to septic loosening. [3]
In total knee arthroplasty, porous tantalum cones are commonly utilised for managing large metaphyseal bone defects, providing biological and mechanical fixation. The cones facilitate the restoration of bone stock and offer a secure foundation for implant fixation in cases of extensive bone loss.
--Spinal Fusion Cages
Tantalum has demonstrated significant potential in spinal fusion surgery, especially as interbody cages used in transforaminal lumbar interbody fusion (TLIF). Tantalum cages are designed to enhance spinal stability and encourage bone integration while minimising the risk of implant subsidence through mechanical compatibility with adjacent bone.
Clinically, osseointegration of tantalum cages has been shown to outperform that of traditional materials such as polyetheretherketone (PEEK). A retrospective evaluation involving 40 patients undergoing TLIF assessed outcomes such as symptom relief, return to normal activities, and radiographic union of fusion. Both groups, featuring metal cages and PEEK cages, exhibited similar improvements in function; however, notable differences were observed in bone response and fusion outcomes. [4]
At one-year follow-up, osteolysis was recorded in 50% of the PEEK cage cases, as opposed to only 10% for the metal cages. Additionally, fusion was observed in 40% of the metal cage cases, significantly better than the 15% seen with PEEK cages. These findings indicate the osteoinductive nature of tantalum, in conjunction with its high biocompatibility and mechanical properties.
2. Dental Implants
The biocompatibility and osseointegration capacity of tantalum are leveraged in dental implants for patients with poor bone quality or those with previously failed implants. Its use is associated with reduced healing time and improved long-term fixation compared to conventional titanium implants.
A preclinical study examined the performance of tantalum Trabecular Metal (TM) dental implants versus traditional titanium screw vent (TSV) implants using a rabbit femoral condyle model. In the study, 20 implants (10 TM and 10 TSV) were randomly inserted in 10 New Zealand white rabbits. Following an 8-week healing phase, the implants were assessed using micro-computed tomography (micro-CT), histology, and histomorphometry. [5]
Results indicated that TM implants performed significantly better than TSV implants in terms of bone-to-implant contact (BIC) and bone volume (BV) within the area of interest. TM implants exhibited a BIC of 57.9% ± 6.5, compared to 47.6% ± 8 for TSV. Similarly, BV measured 57% ± 7.3 for TM implants and 46.4% ± 7.4 for TSV. Micro-CT analysis further corroborated these results, showing the TM group had a bone volume percentage of 89.1% ± 8.7 compared to 79.1% ± 8.6 for the TSV group.
3. Craniomaxillofacial Reconstruction
Porous tantalum plates and meshes are utilised in complex facial reconstructive procedures, providing both aesthetic conformity and mechanical stability. The open pore structure enables soft tissue integration while minimising the risk of infection.
Tantalum exhibits enhanced osteogenic capability compared to conventional materials like Ti6Al4V, making it particularly beneficial for stimulating bone regrowth in the facial and jaw regions.
To address the highly individual nature of craniomaxillofacial (CMF) defects, 3D printing technology has been employed to create patient-specific porous tantalum implants. In a recent study, 3D-printed tantalum scaffolds with nano-topographic surface modifications, achieved through hydrothermal treatment, were evaluated. This surface engineering reportedly enhanced the bioactivity of the scaffold by facilitating osteoblast adhesion and encouraging osteogenic differentiation of bone marrow stem cells (BMSCs). [6]
Conclusion
Porous tantalum has significantly influenced the fields of medicine, particularly in orthopaedic and dental implant surgery. With ongoing advancements in processing and customisation, porous tantalum is likely to remain a fundamental constituent of future implantable biomaterials. For additional tantalum products and technical support, please refer to Stanford Advanced Materials (SAM).
Reference:
[1] Mohandas, Gokhuldass & Oskolkov, Nikita & Mcmahon, Michael & Walczak, Piotr & Janowski, Miroslaw. (2014). Porous tantalum and tantalum oxide nanoparticles for regenerative medicine. Acta neurobiologiae experimentalis. 74. 188-96. 10.55782/ane-2014-1984.
[2] Wang X, Zhou K, Li Y, Xie H, Wang B. Preparation, modification, and clinical application of porous tantalum scaffolds. Front Bioeng Biotechnol. 2023 Apr 4;11:1127939. doi: 10.3389/fbioe.2023.1127939. PMID: 37082213; PMCID: PMC10110962.
[3] Steven H. Weeden, Robert H. Schmidt, The Use of Tantalum Porous Metal Implants for Paprosky 3A and 3B Defects, The Journal of Arthroplasty, Volume 22, Issue 6, Supplement, 2007, Pages 151-155, ISSN 0883-5403.
[4] Cuzzocrea F, Ivone A, Jannelli E, Fioruzzi A, Ferranti E, Vanelli R, Benazzo F. PEEK versus metal cages in posterior lumbar interbody fusion: a clinical and radiological comparative study. Musculoskelet Surg. 2019 Dec;103(3):237-241. doi: 10.1007/s12306-018-0580-6. Epub 2018 Dec 10. PMID: 30536223.
[5] Al Deeb M, Aldosari AA, Anil S. Osseointegration of Tantalum Trabecular Metal in Titanium Dental Implants: Histological and Micro-CT Study. J Funct Biomater. 2023 Jul 6;14(7):355. doi: 10.3390/jfb14070355. PMID: 37504850; PMCID: PMC10382015.
[6] Zhang C, Zhou Z, Liu N, Chen J, Wu J, Zhang Y, Lin K, Zhang S. Osteogenic differentiation of 3D-printed porous tantalum with nano-topographic modification for repairing craniofacial bone defects. Front Bioeng Biotechnol. 2023 Aug 21;11:1258030. doi: 10.3389/fbioe.2023.1258030. PMID: 37671184; PMCID: PMC10475942.

 Bars
Bars
 Beads & Spheres
Beads & Spheres
 Bolts & Nuts
Bolts & Nuts
 Crucibles
Crucibles
 Discs
Discs
 Fibers & Fabrics
Fibers & Fabrics
 Films
Films
 Flake
Flake
 Foams
Foams
 Foil
Foil
 Granules
Granules
 Honeycombs
Honeycombs
 Ink
Ink
 Laminate
Laminate
 Lumps
Lumps
 Meshes
Meshes
 Metallised Film
Metallised Film
 Plate
Plate
 Powders
Powders
 Rod
Rod
 Sheets
Sheets
 Single Crystals
Single Crystals
 Sputtering Target
Sputtering Target
 Tubes
Tubes
 Washer
Washer
 Wires
Wires
 Converters & Calculators
Converters & Calculators
 Write for Us
Write for Us
 Chin Trento
Chin Trento



